Local doctor says current healthcare system is broken
Submitted:
As a physician who has worked in Muskoka since 2003, I feel compelled to write an open letter that has a different perspective and a different narrative than the letters and messages that are being expressed on social and online media. I wanted to take the opportunity to openly share my excitement and my optimism for the newly proposed healthcare model as it provides hope for sustainable delivery of healthcare for all residents and visitors to Muskoka for many years to come.
Throughout my career as a Family Physician, I have fulfilled many roles. I have cared for acute patients in both of the Emergency Rooms here in Muskoka. I have delivered hundreds of babies during my Obstetrical practice that spanned 17 years. Now, I practice Sport and Exercise Medicine so that I can help our communities enjoy active and healthy lifestyles for the past 12 years. My wife, Dr. Deb Harrold, provides in-patient, hospice, and community Palliative Care and was instrumental in establishing Ontario’s first rural residential hospice known as Algonquin Grace here in Huntsville. So the scope of care that we have provided to our community is diverse and has touched and impacted the lives of Muskoka residents from birth through to death.
During our post-graduate residency training in Northeastern Ontario, we had the opportunity to work in most major cities and small rural communities in Northeastern Ontario.
One of the major reasons for deciding to start our medical practices in Muskoka was that there was, and still is,
a genuine sense of collegiality, respect, and professionalism for each other. Healthcare professionals from physicians to nurses, respiratory therapists to diagnostic technicians, everyone worked together in a
patient-centric environment. There was no overarching individualistic “me versus you”, “us versus them”, “I don’t do this”, or “that’s not my job”. Muskoka always had a team-based approach to patient care. Healthcare professionals in Muskoka always joined together to work collaboratively to provide the best possible care for each and every patient who placed their trust and health in the hands of the healthcare team that worked at MAHC.
I emphasize this teamwork and collaborative mindset as we work through this challenging period of healthcare
in Muskoka, where we are presented with a novel model of Muskoka-based healthcare.
I work in our current hospital alongside my physician and healthcare colleagues. We are barely hanging on in a
collapsing healthcare system. We can see that the way we deliver health care locally is no longer viable, nor will it support health care for future generations.
In our current system, services at one hospital get redirected to the other MAHC hospital due to staff shortages or equipment shutdowns. Our inpatient wards are over census leading to admitted patients waiting in beds in the Emergency Room. This overflow situation leads to stress in the emergency departments to provide timely
access to assessment rooms for acutely unwell people. Our current healthcare system is unfortunately mired in issues of staff burned out, staff off on sick or stress leave, managers having to reallocate staff from one area to maintain basic operationality in another area, and frankly the feeling that we are putting out fires while others are burning around us. That is what the status quo is. It is not an enjoyable environment to work in.
However, many of us who provide health care in Muskoka are often asked to dig deep and work extra shifts in various departments where there isn't enough staff to cover them. We are asked to cover for colleagues or those off on medical or stress leave as a result of burnout. All in an attempt to provide our region with seamless care. We, as a team of healthcare professionals, work extremely hard to pull together and make the best of what we get so that the public doesn’t necessarily see how we troubleshoot healthcare and staffing shortages every day to provide seamless care to our region.
The current provision of care in Muskoka is made possible by healthcare providers who are passionate about what we do and the people we serve and care for. We are hanging on for dear life to keep the “status quo” working as we have no other choice. This system is not sustainable, nor are the efforts of the people on the front lines who are providing the care.
The time has come that we need to do something about it. Our local healthcare system needs to change, and we have known for a long time that it needs to change. We have kept putting bandaids on the bumps and scrapes that our system has, but we are now at a breaking point. True innovation and change must take place.
We need to collectively decide in the very near future how we want to see health care delivered moving forward,
and what model of care will deliver it. The government has told us in no uncertain terms that it cannot be status quo because the status quo is a crumbling and failing system. A single site in the middle, or two new identical hospitals in neighbouring communities, is not an option. So we must put these old models behind us, look, and move forward.
As you can see, we are at a point where we have few options left and if we want to provide seamless care to the patients in our region then a regionalized healthcare system needs to be created and adopted.
Regionalized healthcare is collaborative and comprehensive care that is provided at the healthcare facilities in the region and serves the entire region’s population. Healthcare extends beyond the walls of the physical structure of the buildings that provide the care.
Setting up a regionalized healthcare system that works in larger areas but is a novel idea for smaller rural regions, is a bit daunting. It is not something that has a “proven track record of success”. Healthcare providers in Muskoka have never shied away from being on the cutting edge. Rather than pointing out obstacles, we need to look at them as opportunities. We need to focus on the innovative programs and services that this new model may provide to our region. We have the opportunity to be leaders.
It is not fiscally or socially sustainable or responsible to have two rural hospitals in two neighbouring towns providing largely identical services. If our region want to continue to have a robust healthcare system that is truly close to home, we need to be a collaborative organization that, between the two sites and related community programming, we will work together to truly allow for more patients to be cared for “close to home”.
It excites me as a physician that we may be able to offer a more robust healthcare system than what we currently have and a more innovative and sustainable healthcare system than what we currently have.
It is important to note that with this model neither hospital is the “better” hospital. This model is truly a “Muskoka Health Care System” that allows our community members to receive treatment “close to home”.
Not necessarily “closest to their home”, but if Muskoka and the area is home, then care will be close to home.
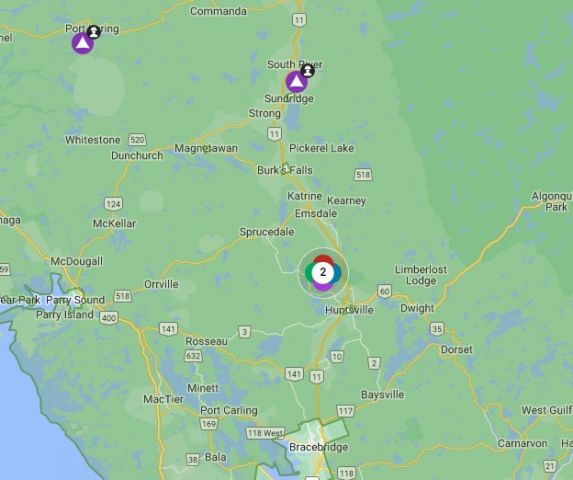
It will allow us to better serve the whole geographic region that MAHC serves. It must be noted that this region
extends well beyond the borders of Muskoka proper in all directions as significant numbers of patients that live in East Parry Sound, Near North as far north as South River, and to the Algonquin Park region access in-patient,
out-patient, surgical, and specialist services in Huntsville and Bracebridge.
Working daily in our current Muskoka healthcare system, I can see how the proposed model will allow us to deliver more care to our patients in a more robust and comprehensive patient-centric care with enhanced medical, surgical, and rehabilitative healthcare services that we already provide because we are centralizing
services at one site or the other. It will allow us to expand the depth of medical, surgical, and diagnostic services that we can offer as a Muskoka Healthcare System. Each hospital, in its own right, will become centres of excellence for the kinds of care that they deliver.
I can see how this model promotes sustainable replenishment of human resources as it will offer us greater
opportunities to recruit physicians, nurses and healthcare providers who want to work in a regionalized healthcare model and not have to work in a large center to do so. Graduating doctors and nurses learn in regionalized healthcare systems in urban areas, and as such they want to work in regions that are forward-thinking, innovative, and work as a collaborative team where the medical support and services are
patient-centric and exist within a regionalized care team.
I can also see the tremendous educational opportunities that lie within this new model offers medical learners. Medical students, residents, and nursing students will be able to learn in concentrated areas of medical and
surgical care interspersed between the two hospital sites. These learners will see how we work collaboratively to provide care as a team of healthcare professionals to our region which is much different than any other rural
community in Ontario. As such, they will see the professional opportunities that exist within this new model of care that will not only be professionally engaging and stimulating but one that will encourage a sustainable
work-life balance.
Developing an innovative solution to our local healthcare crisis is not cheap. This is another reason why I feelthat we need to take this opportunity to change because financial change is possible with a significant contribution by the government who see the potential in not only our healthcare administrators and professionals. This financial opportunity is one that if we don’t take it, it will pass us by and be allocated to a different rural region that is willing to take the risk to make big, bold, and innovative changes.
I, along with others I have had conversations with that are optimistic about this model, know that it will be hard to transition over to the new model of care as it is so different from how our healthcare providers currently work as it is a dramatic change from how we are currently delivering care in Muskoka. The model is proposing that our community residents throughout Muskoka and the surrounding communities we serve will also have to pivot and adapt along with an evolving rural regionalized healthcare system in Muskoka.
So, it won’t just be a challenging period for those of us working in the hospital, but it will be a transformative journey for everyone in our region. A journey that I, as a healthcare provider that is looking towards the future,
will be well worth it in the long run. The transformation of healthcare delivery in our region will finally be able to deliver the care that our Muskoka residents and visitors deserve. Comprehensive care in centers of excellence
that are close to home, where “home” is not the physical address of a patient's house. “Home” is Muskoka. The good thing is that everyone is adaptable. The truth is, that our lives and our communities change every
day. And it changes, we adapt to the new way that we engage with and interact with each other and our community. Health care is no different. To create a sustainable healthcare system for future generations in
Muskoka, we need to dramatically change the way we deliver healthcare, and we as a region will adapt. I am confident that we can do this.
I know it is easy to point out obstacles and identify weaknesses with the current plan. But we can’t simply just point out the challenges and raise questions and then stop there. Nothing productive comes of that. Whatever
the challenge or obstacle that lies in front of us with the current version of the model, we need to collectively look for solutions and move this model forward. I wholeheartedly believe this as a local healthcare provider.
Not only do we need to ask hard and critical questions, identify weaknesses, and find obstacles but, we collectively and collaboratively to look at each and every one of these questions, obstacles, challenges and
weaknesses and find solutions. Solutions that will help shape and mold the model into a sustainable solution that will serve us for many years to come.
While I agree that there are a lot of specific questions surrounding the model, by no means do I think it is a set in stone model. What this model provides us, in my opinion, is an overarching direction that will point the
MAHC Board of Directors and senior administration in a direction where we can build out the future of healthcare delivery in Muskoka. This direction will lead us through a transformative journey of regionalized
rural healthcare delivery in Muskoka. As questions and challenges arise so will opportunities for us as healthcare providers and administration, along with community members, to critically appraise them and then
work together to resolve them with innovative solutions.
We need to dream big, get creative and then implement innovative solutions to make this work. We have to do this for each other as healthcare providers; as patients who receive care in our healthcare system; and for the
sustainability of healthcare for many years to come.
Thank you for taking the time to read this lengthy letter as I felt the need to express my support and optimism for this model. I can only hope that other healthcare providers and community residents who feel the same
way I do take the time to express their support to each other, to the politicians, and to the administration who are working so hard to transform healthcare in Muskoka for the betterment of everyone who lives and visits
here.
Dr. Rich Trenholm
Family Physician, special area of interest in Sport and Exercise Medicine